Hey there! Grab a seat (or your jump bag, whatever’s handy). After 15 years in the field and teaching more paramedic students than I can count, I want to share what’s become my favorite vital sign relationship. And no, it’s not the one between EMS and cold coffee.
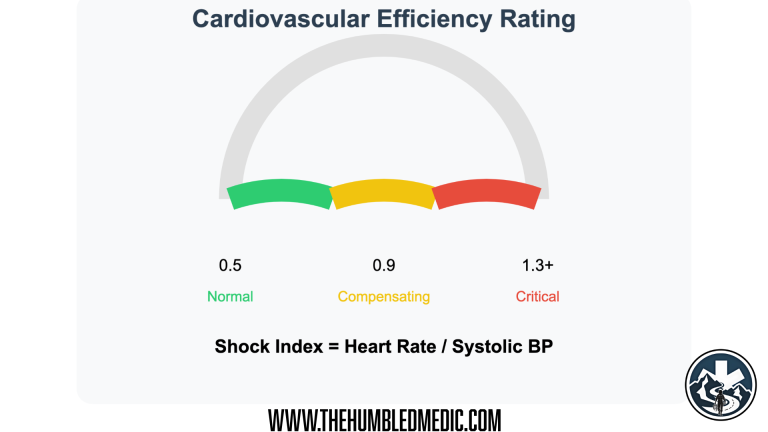
Your patient’s cardiovascular efficiency rating – just like a car’s MPG sticker but way more useful!
Understanding The Numbers: It’s All About Efficiency
Think of the Shock Index like your car’s fuel efficiency. When you’re cruising down the highway at 65 mph with the engine running at 2000 RPM, that’s efficient – you’re getting good speed without working the engine too hard. That’s like a normal Shock Index of 0.7 or less.
When we divide Heart Rate by Systolic Blood Pressure, we’re actually measuring something fascinating – how many heartbeats it takes to generate each “unit” of pressure. It’s like asking, “How hard is the engine working to maintain your speed?”
Normal State:
Engine: 2000 RPM
Speed: 65 mph
Efficient!
Early Strain:
Engine: 4000 RPM
Speed: 65 mph
Working harder for same output…
Critical State:
Engine: 6000 RPM
Speed: 45 mph
Maximum effort, losing ground!
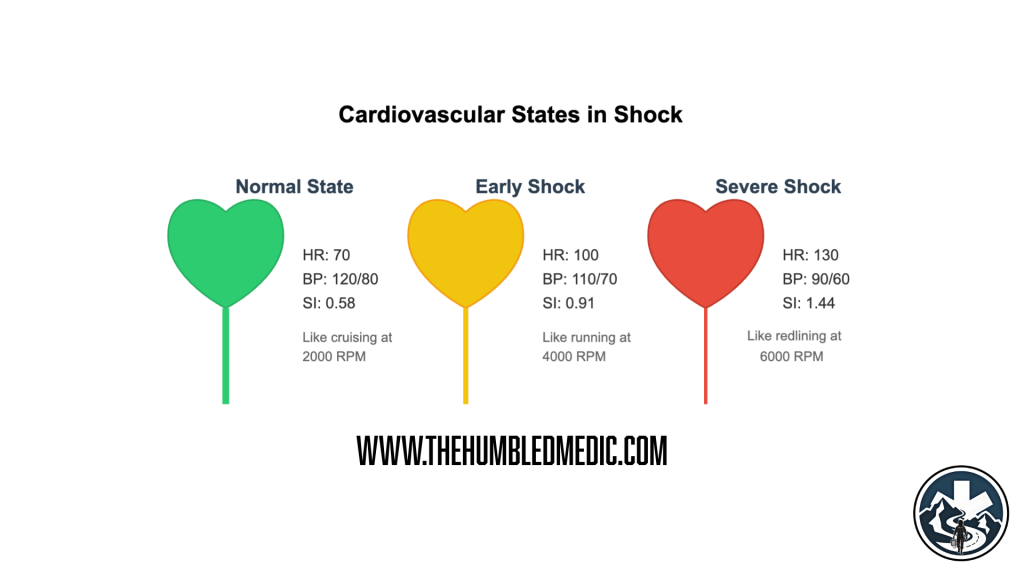
From Theory to Reality: What These Numbers Actually Mean
Let’s break down what we’re really seeing when we calculate that ratio. In a healthy person:
- HR: 70
- BP: 120/80
- Shock Index: 0.58
This means each heartbeat is efficiently generating pressure. Your cardiovascular system is like a well-tuned engine – getting great performance without breaking a sweat.
From “life is good” to “oh snap” in three easy steps
Let me tell you about the call that made me a believer. It was one of those nights – you know the ones – where the coffee’s cold and the dispatch tones are hot. 3 AM, nursing home, elderly patient with “just a fever.”
Initial Assessment:
- HR: 102
- BP: 110/70
- Temp: 38.2°C
- “Looks fine”
- Shock Index: 0.93
That number was telling us something important. This patient’s heart was having to work harder just to maintain baseline pressure. It’s like your engine needing 4000 RPM to maintain the same 65 mph – something’s not right.
Here’s what happens as shock progresses:
Early Shock:
– Heart Rate ↑
– BP maintained
– SI: 0.9-1.2
Think: Engine working harder but maintaining speed
Compensating Shock:
– Heart Rate ↑↑
– BP slightly ↓
– SI: 1.2-1.4
Think: Engine straining, speed dropping
Decompensating Shock:
– Heart Rate ↑↑↑ or dropping
– BP ↓↓
– SI: >1.4
Think: Engine failure imminent
When Numbers Change Actions: Clinical Application Time
Remember that 3 AM nursing home patient? Two hours later, they were in the ICU with septic shock. That Shock Index of 0.93 told us what our gut was trying to say before traditional vital signs showed the whole picture.
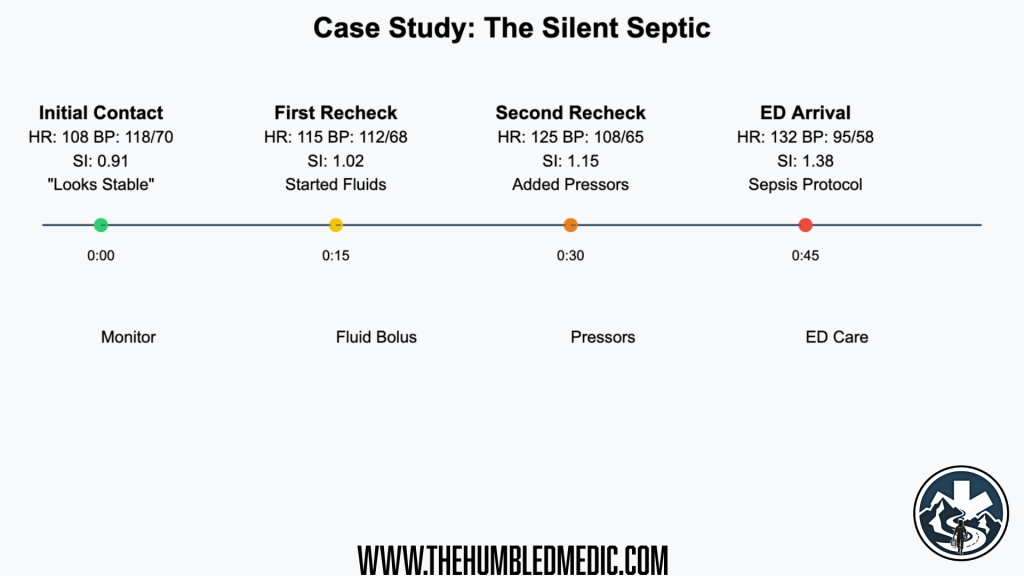
Shows deterioration timeline with intervention points
This is where the Shock Index really shines – it helps us catch things early, when we still have time to act. Let’s talk about what these numbers mean for real-world interventions.
Pre-Intubation: A Story About Why Numbers Matter
Let me tell you about Jake (not his real name) – the case that changed how I approach every intubation. Bad asthma attack, working hard to breathe:
Initial Presentation:
- HR: 122
- BP: 128/80
- RR: 28
- SpO2: 91% on NRB
- Shock Index: 0.95
Now, those vitals might look “stable enough” for standard RSI. But that Shock Index was telling us his body was already working overtime just to maintain those “decent” numbers.
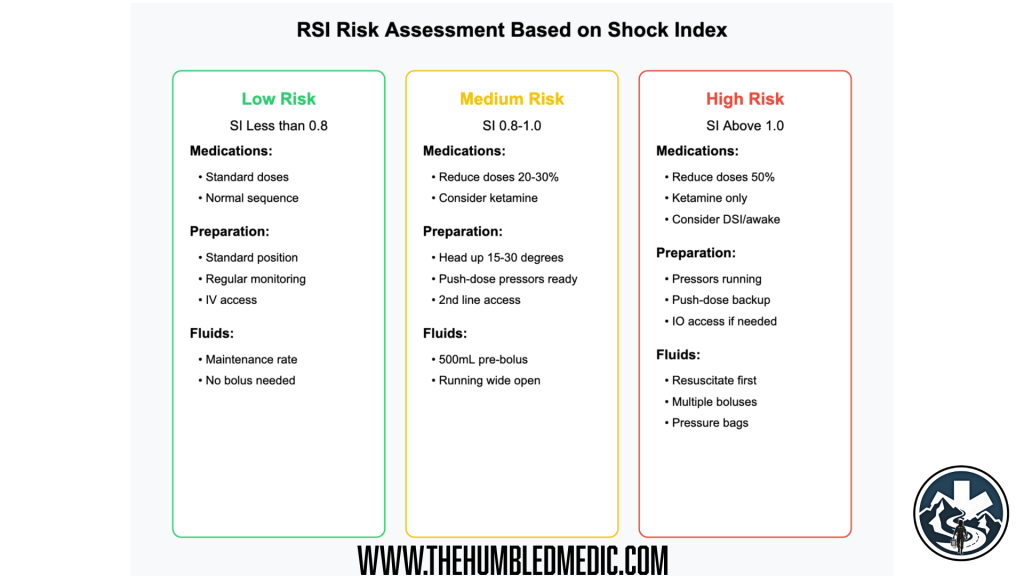
Your “Don’t Kill Your Patient” Guide
Here’s what that number made us do differently:
- Dropped our induction dose by 30%
- Had push-dose pressors drawn up and ready
- Positioned for post-intubation hypotension
- Gave a fluid bolus before we pushed drugs
Ten seconds after tube placement, his pressure dropped to 82/40. But we were ready. Which brings us to our next crucial decision – which pressor to choose?
The Pressor Puzzle: When Numbers Guide Drug Choice
This is where understanding Shock Index patterns really changes the game. Let me introduce you to two patients who taught me everything about pressor selection:
Maria’s Story: The Warm Shock
- HR: 135
- BP: 88/40
- Warm extremities, flash cap refill
- Shock Index: 1.53
- The Setup: Septic shock, vasodilated
Bill’s Story: The Cold Shock
- HR: 89
- BP: 88/40
- Cold extremities, poor cap refill
- Shock Index: 1.01
- The Setup: Post-intubation hypotension, cardiogenic shock
Here’s the thing about push-dose pressors – it’s not just about the numbers, it’s about the pattern. Let’s break down why these patients needed different approaches:
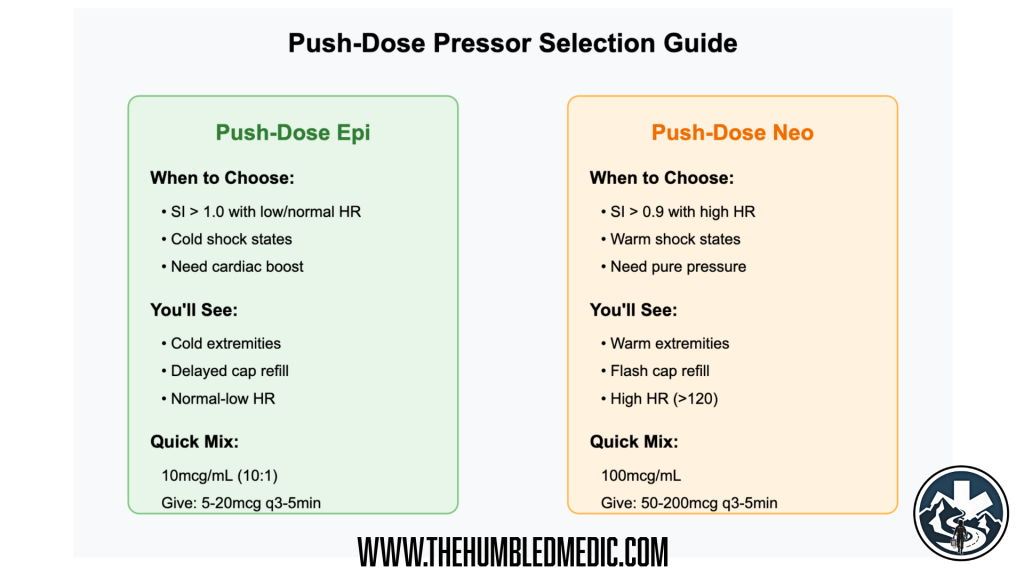
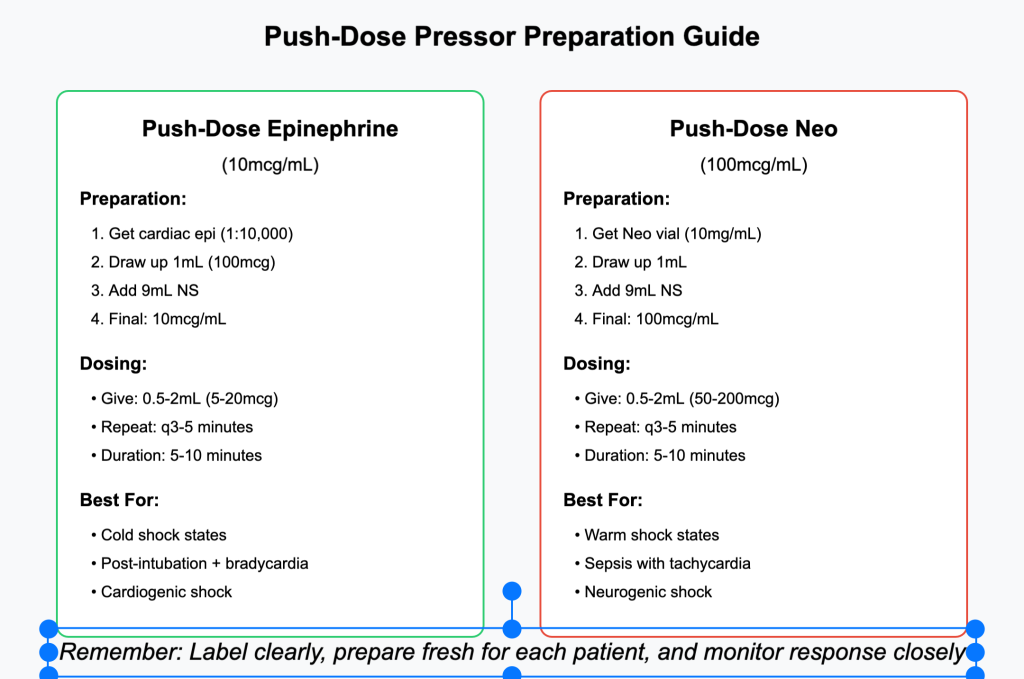
Push-Dose Epinephrine (The Performance Enhancer)
When to use it:
- SI > 1.0 with normal/low HR
- Cold extremities
- Poor cardiac output
- Need for inotropy (heart needs help)
Quick Mix Guide:
- Take cardiac epi (1:10,000)
- Add 9mL NS to 1mL epi
- Now you’ve got 10mcg/mL
- Give 0.5-2mL (5-20mcg) every 5 minutes
Push-Dose Neo (The Tone Restorer)
When to use it:
- SI > 0.9 with high HR
- Warm extremities
- Good cardiac output
- Need for vasoconstriction
Quick Mix Guide:
- 100mcg/mL standard concentration
- Give 0.5-2mL (50-200mcg) every 5 minutes
The Special Populations Plot Twist
Now, just when you think you’ve got this figured out, along comes a pediatric patient or a pregnant woman to change all the rules. Let me tell you about Jenny, age 4, and why she completely changed how I look at pediatric shock indices…
Special Populations: When The Rules Change
Let me tell you about Jenny – 4 years old, three days of diarrhea, and a case that taught me everything about pediatric shock indices.
Initial Vitals:
- HR: 145
- BP: 105/70
- Shock Index: 1.38
In an adult, that SI would have us running for the pressure bags. But kids? They’re playing by different rules.
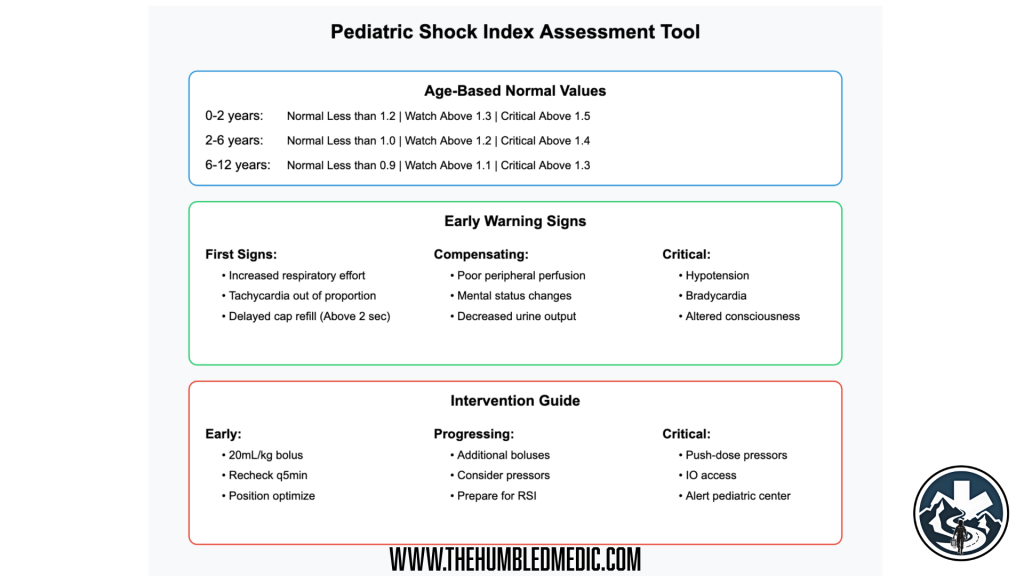
The Pediatric Puzzle
Think of kids like high-performance racing engines – they normally run at higher RPMs, but they’ve got more reserve. Here’s how it breaks down:
Newborn to 2 years:
- Normal SI: < 1.2
- Get Nervous: > 1.3
- Critical: > 1.5
- The Catch: Can lose 30% blood volume before showing obvious tachycardia
2-6 years (like our friend Jenny):
- Normal SI: < 1.0
- Get Nervous: > 1.2
- Critical: > 1.4
- The Catch: Respiratory rate changes often first sign
6-12 years:
- Normal SI: < 0.9
- Get Nervous: > 1.1
- Critical: > 1.3
- The Catch: Watch for increased work of breathing
The thing about kids is they compensate like champions… until they don’t. They’re like that new medic who’s crushing their first few calls – looking great right up until they crash hard.
The Pregnancy Plot Twist
Now let me tell you about Sarah, 32 weeks pregnant, who taught me that pregnancy changes everything – including what shock looks like.
Sarah came in looking “not quite right” at 32 weeks:
- HR: 98
- BP: 122/78
- SI: 0.80
- “Normal” vitals, right? Wrong.
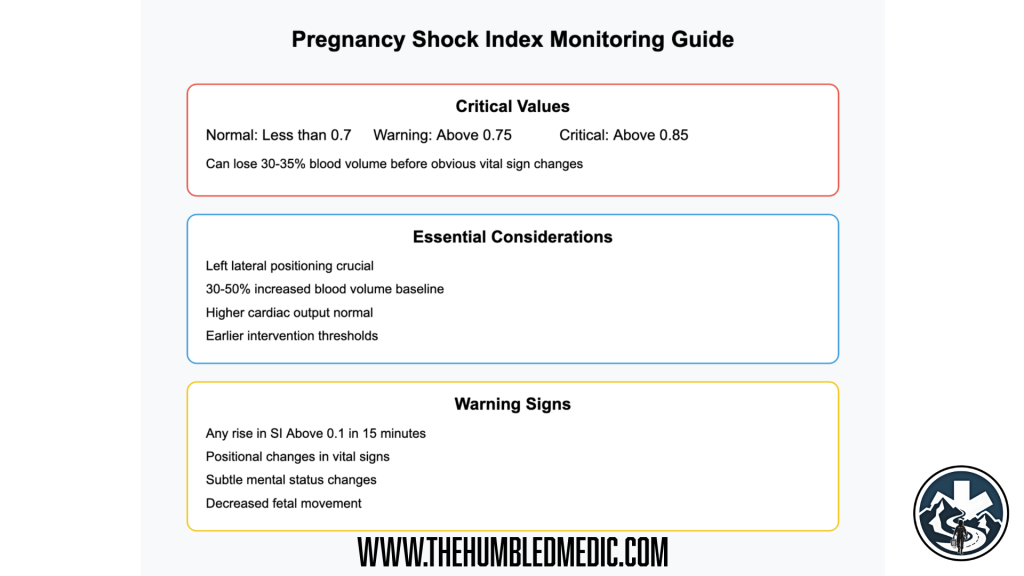
Here’s what pregnancy does to our numbers:
- Normal SI drops to < 0.7
- Get nervous at > 0.75
- Critical at > 0.85
Why? Because pregnancy is like adding a turbocharger to the cardiovascular system:
- Blood volume up 30-50%
- Cardiac output increased
- Different compensatory mechanisms
Sarah’s SI of 0.80 wasn’t just borderline – it was screaming “early shock” in pregnant patient terms. Remember: they can lose 30% of their blood volume before vital signs show obvious changes. By the time they look sick, they’re really sick.
Key Points for Pregnant Patients:
- Left lateral positioning is your best friend
- They compensate great until they crash hard
- That “normal” BP might be actually be low for them
- Watch for subtle signs
The Geriatric Game-Changer
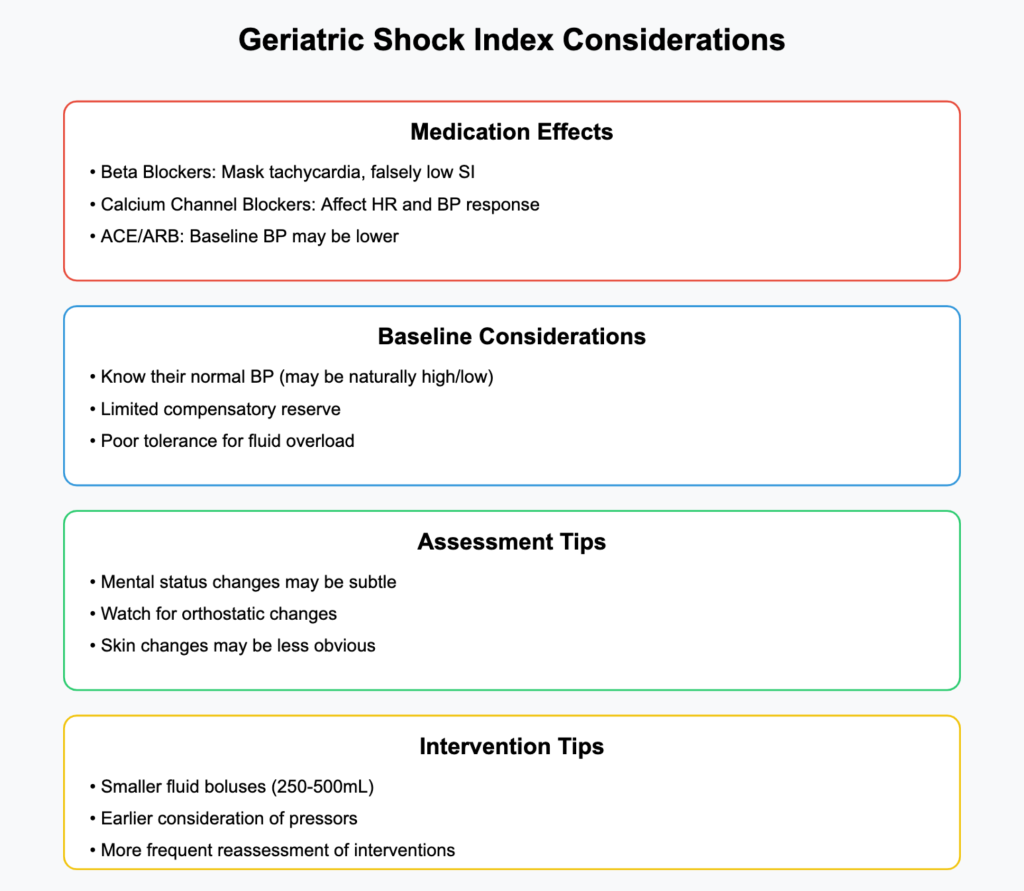
Let me tell you about Frank, 82 years old, who showed me why geriatric shock is like trying to read a book with half the pages missing – the story’s there, but you have to work harder to see it.
Frank’s Initial Vitals:
- HR: 82 (“Good!”)
- BP: 158/90 (“His normal”)
- SI: 0.52 (“Looks fine”)
But Frank was on beta blockers, had chronic hypertension, and his “normal” BP was 180/95. Two hours later, he was in septic shock. Here’s what I learned:
Beta Blockers are like putting a governor on an engine:
- Won’t see the tachycardia
- SI might look falsely reassuring
- Watch the trends more than absolute numbers
Geriatric Vital Sign Interpretation:
- Know their baseline BP
- Compare current SI to their usual
- Look for changes in mentation early
- Temperature changes might be subtle
Clinical Pearls: What 15 Years of “Oh Crap” Moments Taught Me
Let’s talk about pattern recognition – or as I like to call it, “Things I Wish I’d Known Before Learning Them the Hard Way.”
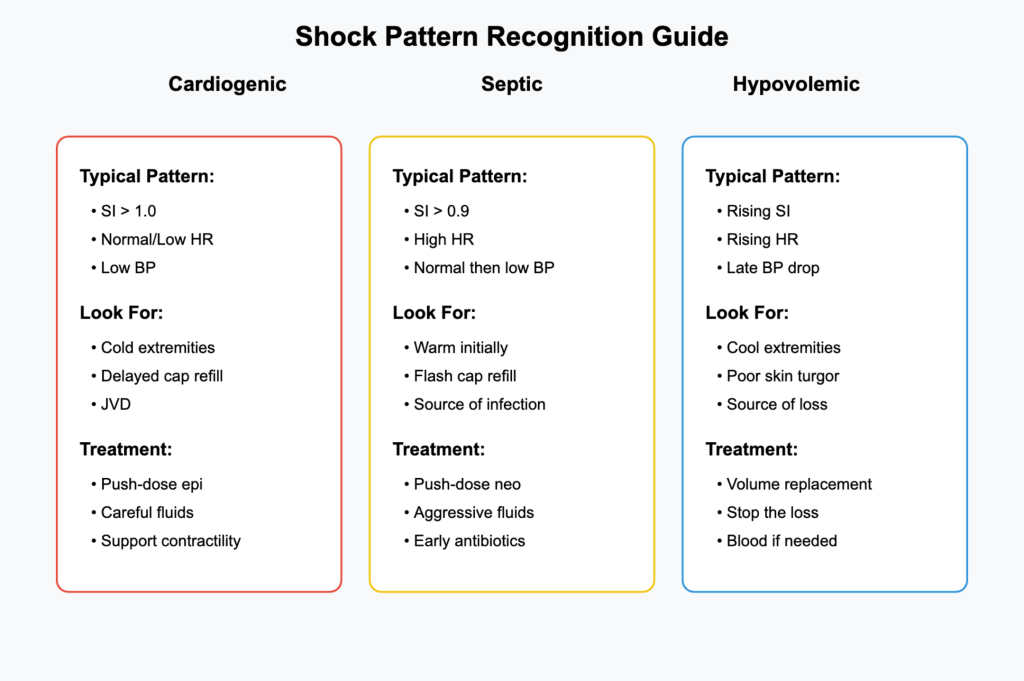
Warm vs Cold: A Tale of Two Shocks
Think of shock patterns like your partner’s coffee preference – knowing the type makes all the difference:
Warm Shock (The Septic Special):
- High SI + warm extremities
- Flash cap refill
- Bounding pulses
- Neo is your friend
- Story: Remember Maria? That’s your template
Cold Shock (The Pump Problem):
- High SI + cold extremities
- Delayed cap refill
- Thready pulses
- Epi might be your play
- Think: Bill’s post-intubation adventure
The Trend is Your Friend
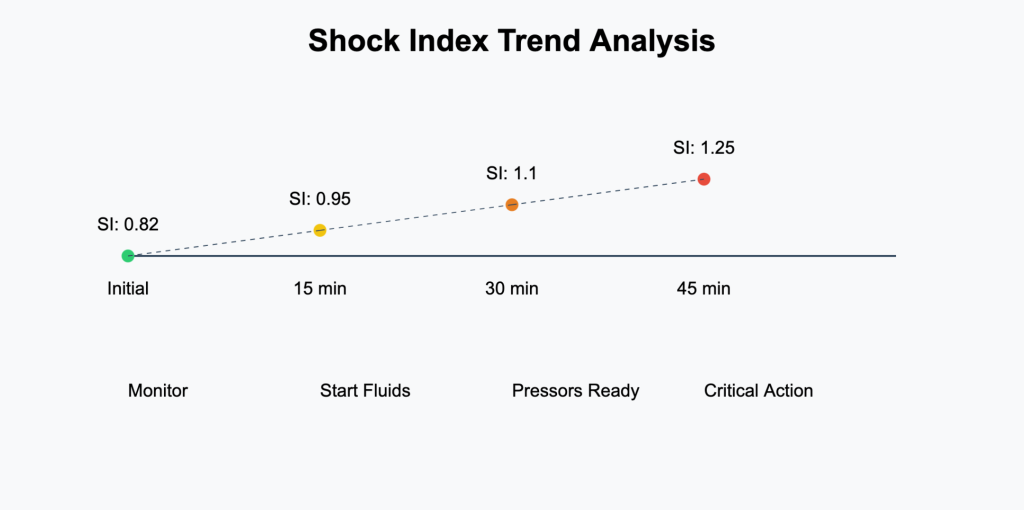
Here’s something they don’t teach you in medic school: it’s not just about the number, it’s about where it’s going. Like that one partner who keeps saying “I’m fine” – you need to watch the pattern:
- Any SI rise > 0.3 in one hour = Bad news
- Improving SI but still cold = Keep watching
- Normal SI but mental status changes = Keep digging
Let me tell you about Tony, my best save of 2023. Started with an SI of 0.82 – not terrible, right? But every 15 minutes it crept up:
- 0.82 → 0.95 → 1.1 → 1.25
- Each bump was trying to tell us something
- By the time we got to 1.25, we were already running fluids and calling ahead
Real World Application: Putting It All Together
Let me take you through three cases that changed how I practice forever. Each one taught me something different about using the Shock Index in real time.
Case 1: “The Silent Septic” Time: 0300 (because isn’t it always?) Initial Vitals:
- HR: 108
- BP: 118/70
- RR: 20
- Temp: 38.2°C
- SI: 0.91
What happened: Every 15 minutes, we recalculated:
- 0315: SI 1.02
- 0330: SI 1.15
- 0345: SI 1.28
The numbers were screaming “sepsis” before the traditional signs showed up. Started fluids early, got antibiotics rolling in the ED within 30 minutes of arrival. That patient walked out of the hospital five days later.
Case 2: “The RSI That Almost Wasn’t” Young asthmatic:
- Initial SI: 0.95
- “Good” BP: 128/80
- Working hard to breathe
[GRAPHIC 16: RSI DECISION MATRIX]
Instead of our usual RSI approach, that SI made us:
- Drop induction doses by 30%
- Pre-load with fluids
- Have push-dose pressors ready
- Position for post-intubation hypotension
Post-tube BP dropped to 82/40, but we were ready. Push-dose neo, fluid bolus, pressure normalized within minutes.
Case 3: “The Pediatric Puzzle” 6-year-old Tommy, three days of “stomach bug”:
Initial Assessment:
- HR: 142 (“He’s just anxious”)
- BP: 105/60 (“Not bad”)
- Cap refill 3 seconds
- SI: 1.35
Here’s where understanding pediatric shock indices saved the day. For his age, that 1.35 wasn’t just high – it was critical. While other providers might have seen “acceptable” vitals, we knew we were looking at early decompensation.
What We Did:
- Immediate fluid bolus
- Early transport decision
- Pre-notification to pediatric center
- Serial SI calculations every 5 minutes
The Outcome: By the time we hit the ED, his SI was 1.48 despite fluids. Turned out to be DKA with severe dehydration. The early recognition and aggressive fluid resuscitation made all the difference.
Quick Reference Tools – Because Nobody Has Time For Math During A Code
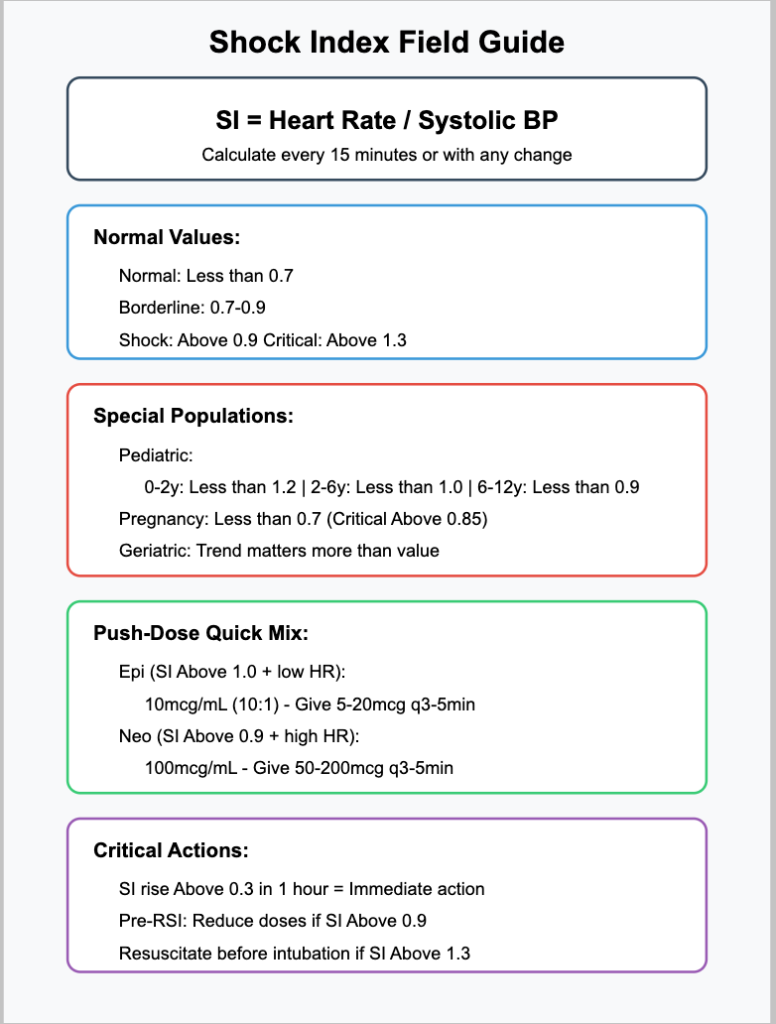
The “Oh Snap” Scale
SI 0.7-0.9: Keep an eye on things
SI 0.9-1.3: Time to work
SI > 1.3: All hands on deck
Pre-Push-Dose Pressor Cheatsheet
Neo (The Pure Pressure Play):
- Mix: 100mcg/mL standard
- Give: 50-200mcg (0.5-2mL)
- Duration: 5-10 minutes
- Best for: High SI + Already Tachy
- Think: “Need squeeze, not speed”
Epi (The Full Court Press):
- Mix: 10mcg/mL (10:1 dilution)
- Give: 5-20mcg (0.5-2mL)
- Duration: 5-10 minutes
- Best for: High SI + Low/Normal HR
- Think: “Need squeeze and speed”
Final Pearls – Things I Learned The Hard Way
- The Magic Minute
- Calculate SI in the first minute on scene
- Recalculate every 15 minutes minimum
- Any change > 0.3 is significant
- Trend is more important than single numbers
- Special Population Secrets
- Pregnant patients: Normal is lower
- Pediatrics: Age changes everything
- Geriatrics: Baseline matters
- Athletes: They compensate longer
- Documentation Tips
- Record initial SI
- Document trends
- Note interventions and responses
- Share calculations with receiving facility
The Bottom Line
After 15 years in the field, here’s what matters most:
- The Shock Index isn’t perfect, but it’s better than guessing
- It catches things early when you still have time to act
- It helps pick interventions that actually make sense
- Most importantly, it’s simple enough to use at 3 AM with no coffee
Remember: A normal Shock Index doesn’t guarantee everything’s fine, but an abnormal one should definitely get your attention. It’s like when your mom used your full name – you knew it was time to pay attention.
Stay safe out there, and keep calculating! Your patients’ cardiovascular systems will thank you.
Disclaimer: Always follow your local protocols and medical direction. This guide is for educational purposes only and should not replace clinical judgment or established guidelines. And remember, if your Shock Index is higher than your coffee intake, you probably have a problem!
References and Further Reading
Core Shock Index Validation Studies
- Rady MY, Smithline HA, Blake H, Nowak R, Rivers E. A comparison of the shock index and conventional vital signs to identify acute, critical illness in the emergency department. Ann Emerg Med. 1994;24(4):685-690.
- Berger T, Green J, Horeczko T, et al. Shock Index and Early Recognition of Sepsis in the Emergency Department: Pilot Study. West J Emerg Med. 2013;14(2):168-174.
Pediatric Applications
- Acker SN, Ross JT, Partrick DA, Tong S, Bensard DD. Pediatric specific shock index accurately identifies severely injured children. J Pediatr Surg. 2015;50(2):331-334.
- Yasaka Y, Khemani RG, Markovitz BP. Is shock index associated with outcome in children with sepsis/septic shock?*. Pediatr Crit Care Med. 2013;14(8):e372-e379.
Pregnancy and Obstetric Applications
- Nathan HL, Cottam K, Hezelgrave NL, et al. Determination of Normal Ranges of Shock Index and Other Haemodynamic Variables in the Immediate Postpartum Period: A Cohort Study. PLoS One. 2016;11(12):e0168535.
Pre-Intubation Risk Assessment
- Heffner AC, Swords DS, Nussbaum ML, Kline JA, Jones AE. Predictors of the complication of postintubation hypotension during emergency airway management. J Crit Care. 2012;27(6):587-593.
Pressor Selection and Shock States
- Kheng CP, Rahman NH. The use of end-tidal carbon dioxide monitoring in patients with hypotension in the emergency department. Int J Emerg Med. 2012;5(1):31.
- Middleton PM, Davies SR. Relationship between mean arterial pressure and end-tidal carbon dioxide in shock. Emerg Med Australas. 2011;23(5):578-586.
Trauma Applications
- Cannon CM, Braxton CC, Kling-Smith M, Mahnken JD, Carlton E, Moncure M. Utility of the shock index in predicting mortality in traumatically injured patients. J Trauma. 2009;67(6):1426-1430.
Geriatric Considerations
- Kim SY, Hong KJ, Shin SD, et al. Validation of the Shock Index, Modified Shock Index, and Age Shock Index in the Korean Emergency Department Sepsis Registry. Am J Emerg Med. 2020;38(1):96-102.
Note: These references represent foundational and current research in Shock Index applications. Always consult current literature and local protocols for the most up-to-date guidelines.