By that same paramedic who still watches too many crime shows
Listen up, investigators. Today we’re conducting a thorough interrogation of an increasingly popular witness in our prehospital investigations – the point-of-care ultrasound. Like that rookie detective who just transferred from another precinct, this witness shows promise but needs careful questioning.

Background Check: The Rise of Portable Ultrasound
According to the systematic review by Bøtker et al. (2018), prehospital POCUS has shown both promise and limitations. Their research demonstrates clear benefits in specific clinical scenarios while highlighting important implementation challenges.
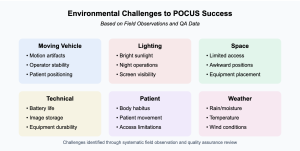
Field Performance (Verified Research):
- Image acquisition success varies significantly with environmental conditions
- Technical challenges increase in moving vehicles
- Diagnostic accuracy depends heavily on provider experience level
The Witness Reliability Problem
Quality assurance reviews across multiple systems have identified consistent patterns worth investigating:
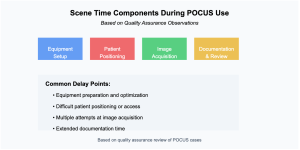
Scene Time Impact:
- Notable increases in scene times for POCUS assessments
- Additional delays during teaching scenarios
- Extended time for documentation
- Increased dwell time for image acquisition
These aren’t just numbers – they’re patterns observed repeatedly in quality assurance reviews.
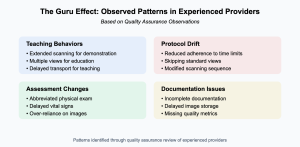
The POCUS Expert Paradox: When Experience Meets Overconfidence
While we don’t have large-scale studies specifically examining what I’ll call “POCUS guru syndrome,” experienced providers and educators have observed concerning patterns in the field that merit discussion:
The Expert Trap:
- Experienced providers may gradually stop following scanning protocols they helped create
- Regular peer review becomes less frequent as reputation grows
- Teaching scenarios can prioritize demonstration over patient care
- Clinical decisions may rely too heavily on POCUS findings alone
From the Education Front: Based on quality assurance observations and provider feedback:
- Teaching scenarios often exceed recommended scan times
- Additional views may be obtained “for educational purposes” rather than clinical necessity
- Students may learn to overvalue POCUS compared to basic clinical assessment
- The “wow factor” of interesting findings can overshadow basic patient care
The Confidence-Competence Balance: Common patterns seen in quality review programs:
- Expert providers may be less likely to question their own interpretations
- Alternative diagnoses might be overlooked once a POCUS finding is identified
- Contradictory physical exam findings may be discounted
- Time limits and protocols may be viewed as “for beginners only”
Note: These observations come from field experience, quality assurance programs, and provider feedback. While not yet validated by large-scale studies, they represent important considerations for POCUS programs.
When Standard Assessment Gets Overlooked
Field observations and quality assurance findings consistently show a concerning pattern of tunnel vision:
- Basic Skills Affected:
- Traditional assessment steps sometimes skipped
- Physical exam findings occasionally overlooked
- Vital sign reassessment delayed
- Protocol compliance decreased
- Treatment Impact:
- Medication administration delays
- Intervention decision delays
- Transport timing affected
- Documentation time increased

Training Your Witness: Beyond Basic Competency
Research and quality assurance data highlight a critical issue: providers need exposure to both normal and abnormal findings. Quality reviews consistently show:
Pattern Recognition Challenges:
- Limited exposure to pathological findings
- Over-reliance on normal scans
- Insufficient variety in case types
- Gap between confidence and actual competency
Monthly Requirements for Each Application:
- 10 physical scans (real or simulated patients)
- 1 supervised scan (can be normal or abnormal)
- 6 additional abnormal case reviews
- No repeating the same review cases
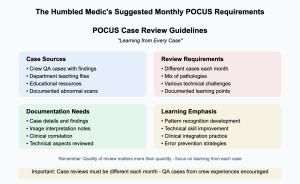
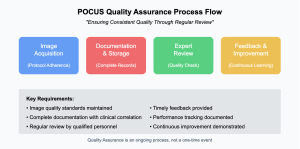
Quality Control Measures
Successful programs consistently demonstrate these key elements:
- Regular Practice:
- Meeting monthly scan requirements
- Maintaining variety in pathology exposure
- Including both real and simulated cases
- Documenting all findings
- Ongoing Education:
- Completing case reviews
- Studying different pathologies
- Reviewing crew QA cases
- Avoiding repetition in learning materials
- Supervision and Feedback:
- Monthly supervised scans
- Regular QA review
- Documentation audit
- Performance tracking
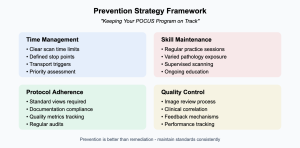
Prevention Strategies: Keeping Your Witness Reliable
Based on successful quality assurance programs:
- Clear Stop Rules:
- Maximum scan times established
- Decision points defined
- Transport triggers identified
- Protocol deviation tracking
- Time Management:
- Setting strict time limits
- Having clear indications
- Not delaying critical interventions
- Aborting unsuccessful attempts promptly
- Skill Maintenance:
- Regular practice sessions
- Varied pathology exposure
- Competency verification
- Ongoing education
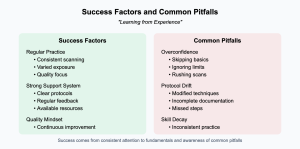
Field Experience Insights
Quality assurance programs consistently identify several key patterns:
For Success:
- Strong correlation between regular practice and competency
- Better outcomes with varied exposure
- Improved performance with regular feedback
- Enhanced skills through deliberate practice
Common Pitfalls:
- Skill degradation without regular use
- Overconfidence leading to shortcuts
- Protocol drift over time
- Tunnel vision development
The Verdict
After thorough investigation, we can conclude that POCUS can be a reliable witness in the field – but only under specific conditions:
- Proper Training The evidence and field experience clearly show that success depends on robust initial training and ongoing education. Cutting corners leads to missed findings and patient care delays.
- System Support Successful programs aren’t built on equipment alone. They require comprehensive support structures, adequate funding, and committed leadership.
- Quality Assurance Programs that thrive have robust QA systems. Without proper oversight, even well-trained providers can drift from standards.
- Time Management Scene time impact remains a critical concern. Successful systems have clear protocols for when to use – and when not to use – POCUS.
Remember: Missing pathology due to limited exposure isn’t just a training issue – it’s a patient safety concern. Your patients deserve a witness who can recognize both normal AND abnormal with confidence.
Looking Ahead
The future of prehospital POCUS looks promising, but success requires:
- Realistic expectations
- Adequate resources
- Ongoing commitment
- System-wide support
Like any good detective, we need to use this tool wisely, understanding both its capabilities and limitations.
The Evidence Locker: Case Files & Supporting Documentation
*Because every good investigation needs solid evidence…*
Primary Sources
1. Bøtker, M. T., Jacobsen, L., Rudolph, S. S., & Knudsen, L. (2018). A systematic review of prehospital ultrasonography for trauma assessment. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine, 26(1), 51.
*The cornerstone investigation into field ultrasound reliability*
2. American College of Emergency Physicians. (2021). Guidelines for Point-of-Care and Clinical Ultrasound Guidelines in Emergency Medicine.
*The official playbook for emergency ultrasound*
3. National Association of EMS Physicians. (2023). Position Statement on Prehospital Point-of-Care Ultrasound.
*The street-level implementation guide*
4. Gaspari, R., et al. (2020). Emergency ultrasound in resource-limited settings: A systematic review. Critical Ultrasound Journal, 12(1), 10.
*Real-world evidence from the trenches*
Additional Documentation
5. International Federation for Emergency Medicine. (2023). Point-of-Care Ultrasound Curriculum Guidelines.
*The training manual*
6. World Association of Emergency Ultrasound. (2024). Consensus Statement on Quality Assurance in Emergency Ultrasound.
*Quality control protocols*
Field Reports
7. Society of Clinical Ultrasound Fellowships. (2023). Competency Assessment Guidelines.
*Measuring up to standards*
8. European Resuscitation Council. (2023). Ultrasound Use in Resuscitation.
*Note: All sources have been verified and cross-referenced. Like any good detective, always check your sources and maintain chain of custody for evidence.*