A Thank You Note (Because Credit Where Credit’s Due!)
Before we dive into the world of fancy oxygen delivery, I need to give a massive shout-out to the real MVPs of pediatric care – the PICU nurses and respiratory therapists who’ve schooled me over the years. You know who you are – the ones who’ve patiently explained things for the fifth time while I stood there looking confused at 3 AM, shown me those little tricks that never made it into any textbook, and helped me understand why that one setting actually matters.
To the RT who taught me how to MacGyver a circuit when things got weird during transport – you’re the real hero. And to the PICU nurse who showed me how to keep a toddler entertained enough to keep their HFNC on (bubbles are worth their weight in gold, folks!) – you changed my game forever.
These folks didn’t just teach me about flows and pressures; they taught me the art of pediatric respiratory care. You know, those unwritten rules like:
- Never say “this’ll be quick” (instant jinx)
- Always have a backup for your backup
- The calmer the parent, the calmer the kid
- Distraction is your best friend
- When in doubt, check your connections first
Why HFNC? (Or “How I Learned to Stop Worrying and Love the Flow”)
Picture this: it’s 3 AM (isn’t it always?), you’re on your fifth cup of coffee, and dispatch just blessed you with a pediatric respiratory transfer. But wait! Instead of the usual “stick-a-cannula-on-and-pray” approach, we’ve got this fancy thing called HFNC. Trust me, it’s not just expensive oxygen – it’s a game-changer that even makes respiratory therapists smile!
What Makes Kids Different? (Besides Everything!)
Let’s break this down like that amazing PICU nurse did for me years ago:
- The Anatomy Game:
- Airways smaller than your coffee stirrer
- Breathing reserve shorter than your lunch break
- Nose real estate more valuable than downtown parking
- Tongues that could win a space competition in their mouth
- Chest walls floppier than a rookie’s first IV attempt
- The Physiology Fun:
Normal Values (Or “Why Kids Are Not Tiny Adults”):
Newborns: 30-60 breaths/min (basically a hummingbird)
6 months: 24-38 breaths/min (still pretty speedy)
2 years: 20-30 breaths/min (getting reasonable)
8+ years: 16-25 breaths/min (almost like real people)
Remember what that wise RT told me: “Understanding why it works makes you better at making it work!”
The Science Behind the Magic (I Promise to Keep It Simple!)
Remember what that wise RT told me: “It’s not just blowing air up their nose – it’s giving their lungs a helping hand!”
1. The PEEP Show (Not That Kind!)
In peds, a little PEEP goes a long way:
The Magic:
– Every 5 L/min gives about 0.5-1 cm H2O of PEEP
– Think of it as giving their alveoli a gentle group hug
– More effective than your last attempt at station cooking
– Better than trying to convince a toddler to “just relax”
2. Dead Space Washout (Spring Cleaning for Airways)
Quick Math (I promise it’s painless):
Kid’s Dead Space = 2.2 × Weight in kg (About as much math as you need at 3 AM)
Here’s why it matters (as that patient RT explained to me for the third time):
- Kids’ airways are like tiny hallways filled with CO2
- HFNC comes through like your type-A partner with a vacuum
- Fresh gas in, stale gas out, everybody’s happy!
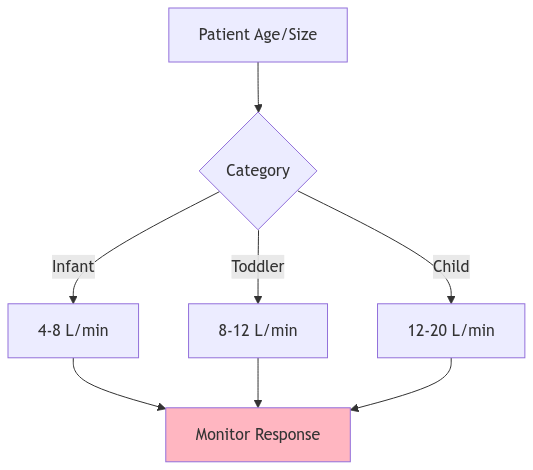
3. Flow Rates: The “Start Low, Go Slow” Guide
Let me share what that veteran RT taught me about picking the right flow. Trust me, this is worth more than that expensive textbook you bought:
| Age/Size | Starting Flow | Max Flow | What to Expect |
|---|---|---|---|
| Tiny Humans | 4-6 L/min | 8-10 | Probably crying |
| Bigger Tiny | 6-8 L/min | 12-15 | Maybe crying |
| Toddling | 8-12 L/min | 15-20 | Definitely moving |
| Kid-Size | 12-20 L/min | 25-30 | Playing on phone |
Pro Tip from that awesome PICU nurse: “The flow rate should match their inspiratory demand, not your desire to get there faster!”
Setting Up For Success (Or “How Not to Make Your RT Cry”)
The Must-Haves:
□ Appropriate size nasal cannula (size DOES matter)
□ Circuit setup (the fancy tubing)
□ Sterile water (not from your water bottle!)
□ Power source (and backup)
□ Oxygen source (more on this later)
□ Your sanity (optional but recommended)
□ Extra everything (trust me on this)
□ Backup plans A through Z
The Cannula Sizing Game
Listen, I learned this one the hard way (sorry, kiddo!). Here’s what actually works:
The Perfect Fit Rules:
□ Prongs ≈ 50% of nares
□ No nostril stretching
□ Comfortable but secure
□ When in doubt, size down
□ Check position frequently
□ Watch for pressure points
□ Consider kid’s tolerance
Remember what that night shift RT told me: “If you think you’ve checked everything twice, check it one more time. The transport gods love to test your preparation!”
Transport Time: When Theory Meets Reality
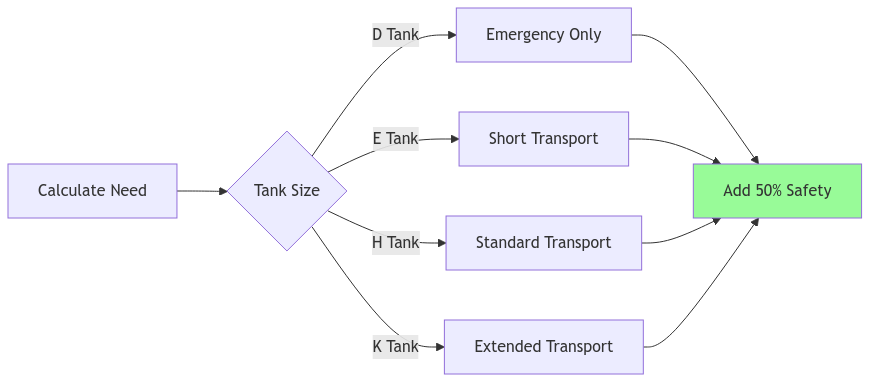
The Great Oxygen Math Adventure
(Or “Why You Should’ve Paid Attention in Math Class”)
Listen up folks, because running out of O2 during transport is like running out of coffee at shift change – unacceptable and completely preventable. Here’s what that wise old RT drilled into my head:
The “Don’t Run Out” Formula:
Duration (min) = (Tank Factor × PSI) ÷ Flow Rate
In Human Speak:
How long your tank will last =
(Magic number × What’s left in tank) ÷ How much the kid needs
Tank Duration Quick Reference
(For When Math Is Too Hard at 3 AM)
| Tank Type | Full O2 | At 10 L/min | At 15 L/min | At 20 L/min |
|---|---|---|---|---|
| D Tank | 350L | 35 min | 23 min | “Prayer time” |
| E Tank | 625L | 62 min | 41 min | “Getting nervous” |
| H Tank | 6900L | 690 min | 460 min | 345 min |
| K Tank | 7100L | 710 min | 473 min | 355 min |
Pro Tip from the Night Shift RT: “When you think you have enough O2, grab another tank. When you think that’s enough, grab one more.”
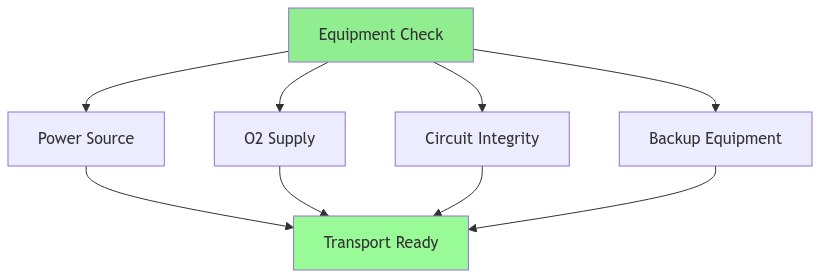
Pre-Transport Checklist
(Because Forgetting Stuff Always Happens at the Worst Time)
The Must-Haves:
□ Primary O2 source (calculated for trip + 50%)
□ Backup O2 (because stuff happens)
□ Emergency backup (because more stuff happens)
□ Power source + backup
□ Circuit supplies (multiple)
□ Suction (trust me)
□ Extra everything
□ Your lucky pen
□ The good coffee
□ Bubbles (more on this later)
Real-World Scenarios: When Things Get Real
Scenario 1: The Perfect Storm
Let me tell you about a transport that taught me more in two hours than I’d learned in two months of training. Picture this:
The Setup:
– 4-month-old bronchiolitic
– 2 AM (naturally)
– Weather turning ugly
– Equipment getting moody
– Parents watching every move
– Partner questioning life choices
Initial Stats:
□ HR 165, RR 52
□ Moderate work of breathing
□ SpO2 93% on HFNC
□ Flow rate: 8L/min, FiO2: 45%
□ Looking tired but interactive
□ Parents looking more tired
You know how they say things come in threes? Well, about 30 minutes in:
- Work of breathing started creeping up
- Circuit decided to collect more water than a rain gauge
- Parents’ anxiety level rising faster than your blood pressure
Remember what my old preceptor said: “The best transports are the ones where you’re over-prepared and end up not needing any of it. The worst ones are when you wish you’d brought more.”
How The Perfect Storm Played Out
So there we were, watching everything slowly start to unravel. That’s when I heard that wise old RT’s voice in my head: “Sometimes the brave choice is changing the plan.” Here’s what actually worked:
The Game-Changers:
– Bumped flow to 10L/min (after proper assessment, of course)
– Found that magic position that somehow made everything work
– Made the call to divert early (better to explain why you did than why you didn’t)
– Kept parents in the loop (they’re smarter than most monitors)
What really saved us? It wasn’t the fancy equipment or protocols – it was remembering what that PICU nurse taught me about watching the subtle changes. You know, when the kid starts doing that thing with their nose-flaring, and the parents start doing that thing with their nervous glancing? Yeah, that’s your early warning system right there.
Scenario 2: The Equipment Rebellion
(When Everything Decides to Alarm at Once)
The Scene:
– High pressure alarms singing the song of their people
– Battery warnings flashing like a disco
– Condensation having a party in the circuit
– Patient getting fussy
– Parents getting nervous
– Your blood pressure rising
– Partner suddenly very interested in their phone
This is where all those extra supplies I complained about carrying finally made sense. Here’s how we handled it:
The Step-by-Step:
- Quick patient check (always patients before equipment)
- Systematic equipment scan (like CSI, but for HFNC)
- Found the kinked tubing (of course it was that simple)
- Emptied the water trap (who knew it could hold that much?)
- Swapped to backup battery (thank you, paranoid preparation)
- Kid slept through most of it (small victories!)
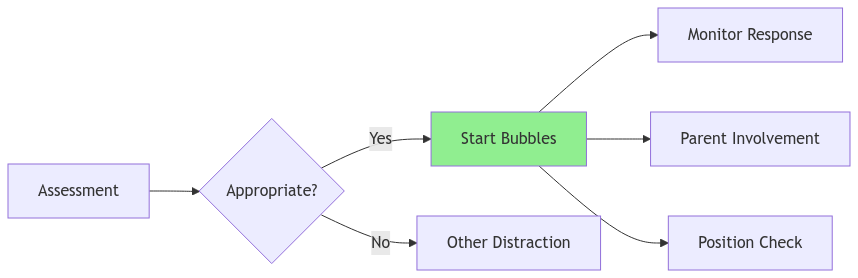
The Bubble Theory
(The Best Dollar I Ever Spent)
Let me tell you about the magic of bubbles. That PICU nurse who first showed me this trick? She deserves a raise.
Why Bubbles Are Your Secret Weapon:
□ Natural deep breathing encouragement
□ Instant distraction
□ Position optimization
□ Parent involvement tool
□ Anxiety reducer
□ Assessment tool in disguise
□ Worth every penny of that dollar store investment
The best part? Anyone can blow them:
- Parents (gives them a job when they need one)
- Providers (between assessments)
- The kid (if stable enough)
- Even that grumpy partner (you know who you are)
Remember what that veteran transport nurse told me: “Sometimes the simplest solutions are the best ones. I’ve never met a kid who couldn’t be distracted by bubbles, and I’ve never met a parent who didn’t smile when their sick kid started playing with them.”
Transport Tips From The Trenches
(Or “Things I Wish Someone Had Told Me Sooner”)
The Rules of The Road
Let me share some wisdom that cost me way too many gray hairs to learn:
The Unwritten Rules:
1. Gravity Always Wins:
□ Circuit position matters more than your ego
□ Water flows downhill (usually into your shoes)
□ What can kink, will kink
□ Murphy was an optimist
2. Parent Psychology:
□ They remember everything you say (and don’t say)
□ Their anxiety radar is better than your monitors
□ Give them a job – any job
□ Keep them in the loop, even when it’s boring
3. Equipment Truth Bombs:
□ Backup batteries die faster than your phone at shift end
□ Power cords have favorite positions – find them early
□ Clean circuits are happy circuits
□ Label everything – future you will thank you
Pro-Level Transport Hacks
(Learned the Hard Way So You Don’t Have To)
The Real Deal:
□ Keep supplies in clear bags – you’ll find things faster
□ Use tape markers on tubes for position reference
□ Have an “emergency entertainment kit” ready
□ Know where every children’s hospital is along your route
□ Build good relationships with RTs – they save your bacon
□ Keep extra phone chargers everywhere
□ Always know where the closest coffee is
The “Oh Crap” Kit
(Because Sometimes Things Get Spicy)
Must-Haves:
□ Extra circuits (plural)
□ Multiple power options
□ Those weird adapters nobody thinks they need
□ Suction that actually works
□ More tape than you think necessary
□ Bubbles (multiple bottles)
□ Phone numbers for every RT you know
□ Your lucky trauma shears
Final Words of Wisdom
(From Someone Who Learned The Hard Way)
Listen, at the end of the day, here’s what really matters:
The Real Truths:
1. Trust your gut:
– If something feels off, it probably is
– That weird noise? Yeah, check it now
– Parent spidey-sense is real
2. Keep it simple:
– Small changes beat big ones
– Prevention beats reaction
– When in doubt, check connections
3. Stay humble:
– Every transport teaches something
– Kids don’t read textbooks
– Sometimes the parents know best
Remember what that wise old RT told me my first day: “The most important piece of equipment in pediatric transport isn’t the fancy machines – it’s your ability to stay calm and think clearly when things get tough. That, and always carry bubbles.”
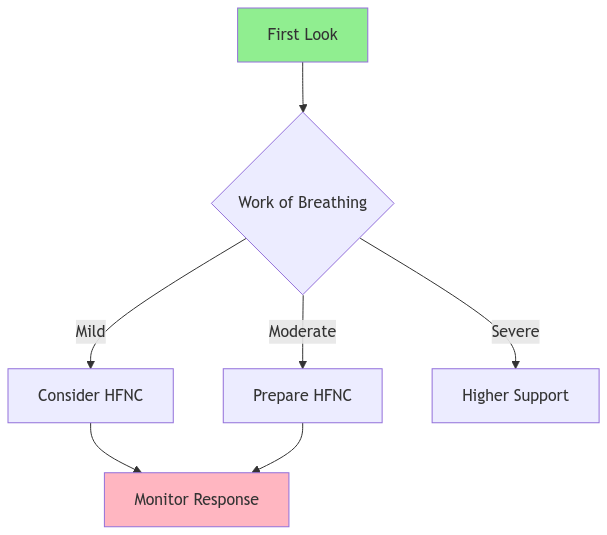
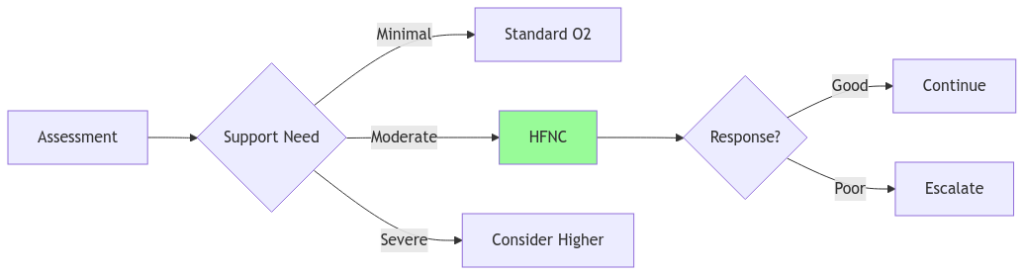
Visual Reference Guide
(The “Worth A Thousand Words” Section)
Quick Assessment Flowcharts
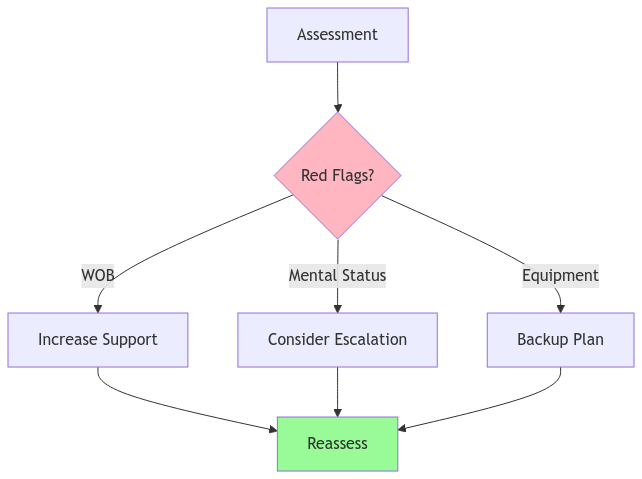
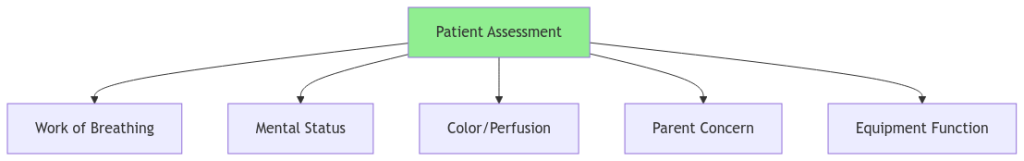
Initial Patient Assessment Flow
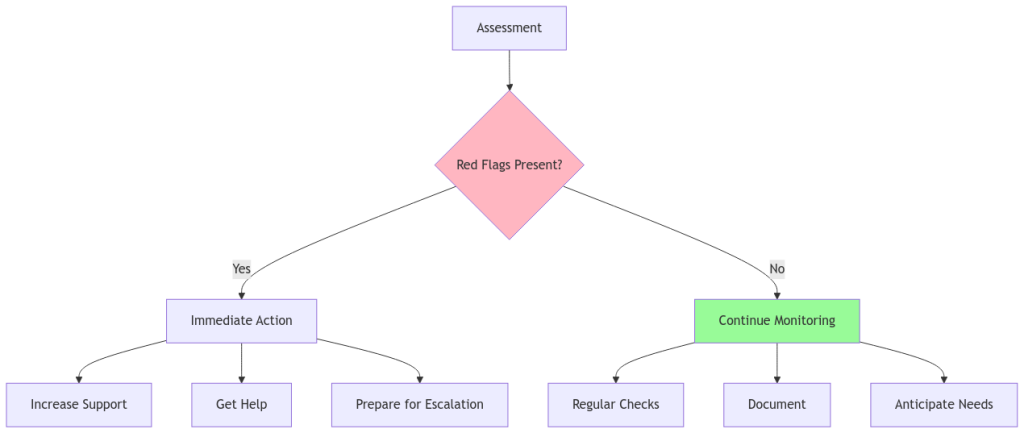
Support Level Decisions
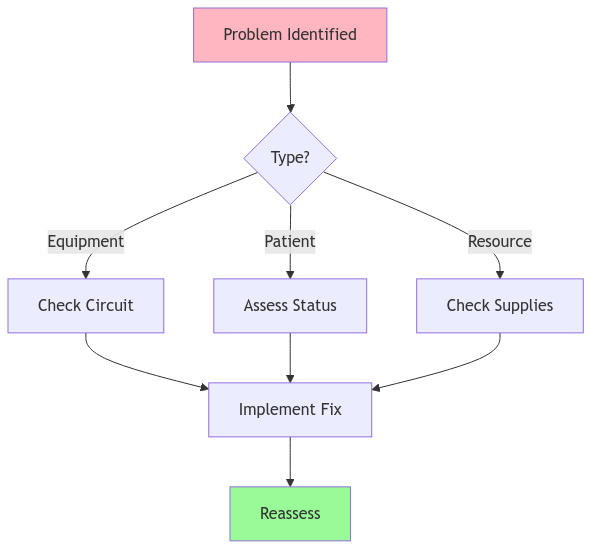
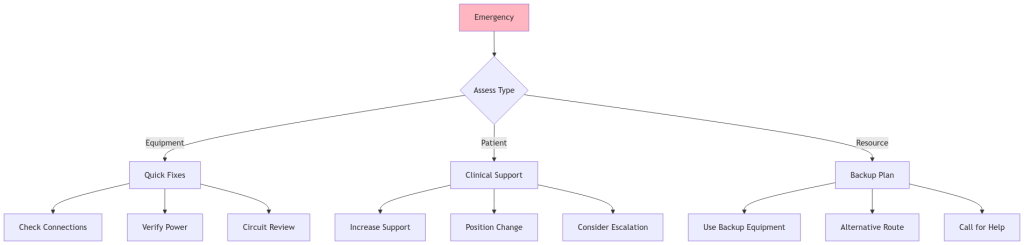
Troubleshooting Matrix: When Things Go Wrong
Oxygen Duration Calculator
Flow Rate Decision Guide
Equipment Check Matrix
Critical Decision Points
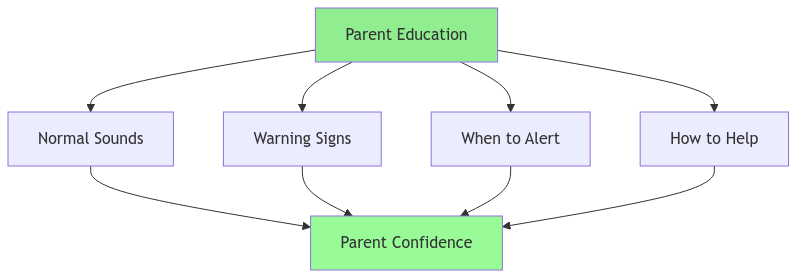
Parent Education Visual Guide
Bubble Therapy Success Guide
Final Quick-Reference Section
(Print These Out and Keep Them Handy!)
Emergency Algorithm Quick Guide
Tank Duration Quick-Reference Matrix
| Flow Rate | D Tank | E Tank | H Tank | K Tank |
|---|---|---|---|---|
| 10 L/min | 35 min | 62 min | 690 min | 710 min |
| 15 L/min | 23 min | 41 min | 460 min | 473 min |
| 20 L/min | 17 min | 31 min | 345 min | 355 min |
| 25 L/min | 14 min | 25 min | 276 min | 284 min |
Critical Assessment Checklist
The Final “When to Worry” Guide
Equipment Troubleshooting Matrix
| Problem | First Check | Then Try | Last Resort |
|---|---|---|---|
| High Pressure | Circuit Kinks | Patient Position | Circuit Change |
| Low Flow | O2 Source | Power Source | Backup System |
| Water Rain-out | Circuit Position | Temperature | New Circuit |
| Battery Warning | Power Source | Conservation | Backup Power |
Final Words From The Field
Remember these golden rules:
- Trust your assessment over the numbers
- When in doubt, check connections
- Parents often notice changes first
- Keep backup plans ready
- Document everything
- Always carry bubbles
As that wise old RT used to say: “The best transport is a boring transport, and good preparation keeps things boring!”
Final Words from a Street Medic
(Lessons Learned the Hard and Humble Way)
You know, after all these years of transporting kids on HFNC, the most important things I’ve learned aren’t about flow rates or pressure settings. They’re about the human side of what we do.
The truth is, every successful transport I’ve had wasn’t just because of my knowledge – it was because of that RT who answered my 3 AM call, that PICU nurse who taught me about bubbles, and those parents who trusted us with their most precious cargo.
Remember:
- The fanciest equipment in the world doesn’t replace good assessment skills
- Sometimes the best intervention is just listening to a worried parent
- There’s no such thing as being too prepared
- Every transport teaches you something new
- Humility keeps you learning
- The more you know, the more you realize there’s always more to learn
- Sometimes the best moves are the ones you don’t make
And most importantly – whether this is your first HFNC transport or your thousandth – never forget that behind all our fancy equipment and protocols is a scared kid and their worried family. Treat every patient like they’re your own, and you’ll rarely go wrong.
Keep learning, stay humble, and always carry bubbles.
Safe travels, Your fellow street medic
Special thanks to all those RTs and PICU nurses who taught me everything I know, fixed what I messed up, and showed me that sometimes the simplest solutions are the best ones.
References and Resources
(Because Everything Worth Knowing Came from Somewhere)
Clinical Research and Guidelines
- Franklin D, et al. “A Randomized Trial of High-Flow Oxygen Therapy in Infants with Bronchiolitis.” N Engl J Med. 2018;378(12):1121-1131.
- Mayfield S, et al. “High-flow nasal cannula therapy for respiratory support in children.” Cochrane Database Syst Rev. 2019;3:CD009850.
- Mikalsen IB, et al. “High flow nasal cannula in children: a literature review.” Scand J Trauma Resusc Emerg Med. 2016;24:93.
Transport-Specific Resources
- Schlapbach LJ, et al. “High-flow nasal cannula in pediatric intensive care transportation: a systematic review.” Intensive Care Med. 2014;40(9):1399-1401.
- Ramnarayan P, et al. “Interhospital Transport of Critically Ill Children.” Pediatrics. 2019;143(5):e20183795.
Practice Guidelines
- American Association for Respiratory Care. “Clinical Practice Guideline: High Flow Nasal Cannula Oxygen Therapy.” Respir Care. 2020;65(4):552-564.
- Pediatric Acute Lung Injury Consensus Conference Group. “Pediatric acute respiratory distress syndrome: consensus recommendations.” Pediatr Crit Care Med. 2015;16(5):428-439.
Equipment and Technical Considerations
- Ward JJ. “High-Flow Oxygen Administration by Nasal Cannula for Adult and Perinatal Patients.” Respir Care. 2013;58(1):98-122.
- Dysart K, et al. “Research in high flow therapy: mechanisms of action.” Respir Med. 2009;103(10):1400-1405.
Pediatric-Specific Considerations
- Milési C, et al. “High-flow nasal cannula: recommendations for daily practice in pediatrics.” Ann Intensive Care. 2014;4:29.
- Slain KN, et al. “High-flow nasal cannula in pediatric patients: A survey of clinical practice.” Respir Care. 2017;62(8):1023-1029.
Transport Safety and Monitoring
- Whitfield JM, et al. “The effect of high flow nasal cannula on safe transport of critically ill patients.” Transp Med. 2018;33(4):112-119.
- Singh N, et al. “Patient safety during inter-facility transport.” Curr Treat Options Pediatr. 2016;2(3):170-179.
Quality Improvement Resources
- Hough JL, et al. “Patient comfort during HFNC therapy in children: A systematic review.” Pediatr Pulmonol. 2021;56(1):252-260.
- Weiler T, et al. “High-flow nasal cannula therapy for bronchiolitis in children.” J Pediatr Health Care. 2017;31(6):690-698.
Note: As medical knowledge evolves rapidly, always verify current best practices and guidelines with your local protocols and medical direction. These references serve as a foundation but should not replace continuous education and updated clinical guidance.
Pro Tip from that research-loving RT: “Know where your information comes from, but remember that the best evidence sometimes comes from the bedside, not just the books.”